We empower healthcare revenue cycle management through efficient collaboration, transparency and drafting tailored solutions for independent providers, specialty groups, and urgent care centers.
Achieve financial stability with AllegianceRCM’s tailored RCM solutions. From denial management to credentialing, we streamline your revenue cycle and provide insights to drive sustainable growth for your practice.


We are technology agnostic and have worked on all modern SaaS based electronic medical records and practice management systems. The following is a list of most common practice management systems used across the industry and extensively used by us. If you don’t see your EHR here, please contact us.














Healthcare providers often face revenue inefficiencies, claim denials, and cash flow challenges. At AllegianceRCM, we take a different approach crafting tailored strategies to reduce AR days, improve claim approvals, and streamline billing, ensuring your financial success.
OUR SERVICES

We focus on maximizing revenue through efficient RCM processes and transparent reporting, providing actionable insights to optimize financial performance and drive growth.
SPECIALTIES WE SERVE
WHO WE ARE
Since 2007, our team has been empowering healthcare providers with innovative, efficient revenue cycle solutions. Our tailored, research-driven approach simplifies operations, maximizes reimbursements, and drives practice success. From cutting-edge technology to full-service billing, we create solutions that grow with your needs.
We are technology agnostic and have worked on all popular payers including Medicaid, Medicare and Most of commercial payers across various states. The following is a lists most common payers and tools used across the industry and extensively used by us. If you don’t see your payer here, please contact us.




























Transform your online presence with custom healthcare websites designed to attract, engage, and convert. Leveraging our deep knowledge of healthcare and revenue cycle management, we craft professional, user-friendly websites that reflect your practice’s expertise, build trust with patients, and drive measurable results.
TESTIMONIALS
We understand that choosing the right revenue cycle partner is a critical decision for your practice. That’s why we’ve compiled answers to the most common questions we receive from healthcare providers.
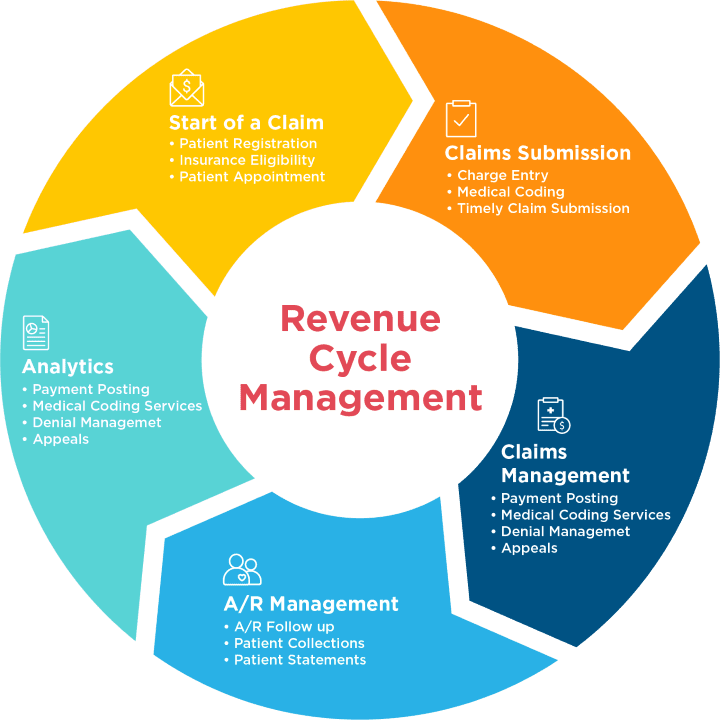
AllegianceRCM provides comprehensive revenue cycle management (RCM) services, including medical billing, coding, claims processing, denial management, insurance verification, patient collections, compliance audits, and financial reporting. We also offer provider credentialing, workforce extension, virtual assistance, and white-label RCM solutions to help healthcare organizations streamline operations and maximize reimbursements.
AllegianceRCM partners with a wide range of healthcare providers, including private practices, specialty clinics, ambulatory surgery centers (ASCs), hospitals, urgent care centers, behavioral health providers, and medical billing companies. We also support EHR and practice management companies through white-label RCM solutions tailored to their business needs.
We use a combination of AI-driven automation, certified coders, and rigorous quality checks to ensure claim accuracy and timely submission. Our pre-submission claim scrubbing, coding audits, and payer-specific compliance checks reduce denials, while our proactive follow-ups help accelerate reimbursements and minimize revenue leakage.
We provide real-time access to financial reports, claim status, reimbursement trends, and denials analysis through a secure client portal. Our customized reporting, scheduled performance reviews, and data-driven insights help providers track revenue cycle efficiency, identify bottlenecks, and make informed decisions to optimize cash flow.
AllegianceRCM improves cash flow by reducing claim denials, accelerating reimbursements, optimizing patient collections, and ensuring accurate coding and documentation. Our insurance eligibility verification, automated billing workflows, and payer negotiations help providers capture every dollar they’re owed while minimizing outstanding accounts receivable.

AllegianceRCM is a trusted leader in revenue cycle management, delivering tailored solutions for healthcare providers, including independent practices, specialty groups, and urgent care centers. Our expertise in medical billing, coding, denial management, and credentialing ensures streamlined operations and maximized reimbursements. With a commitment to transparency, cutting-edge technology, and personalized service, we empower providers to focus on patient care while achieving financial success. At AllegianceRCM, your practice’s growth is our priority.
© 2024 I allegiancercm.com