Ensuring timely provider credentialing and enrollment is critical to maintaining a steady revenue flow. At AllegianceRCM, we streamline the entire process—from payer applications to ongoing compliance—reducing administrative burdens and securing faster approvals. Our expert-driven approach ensures your providers are fully credentialed and enrolled with the right payers, minimizing denials and revenue disruptions.
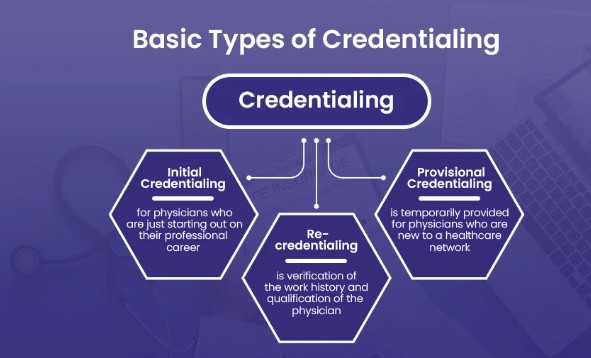
Provider credentialing and enrollment are fundamental to establishing a healthcare provider’s eligibility to bill payers. Any delays or errors in this process can lead to claim denials, delayed payments, and compliance risks.
How We Help You Succeed.

At AllegianceRCM, we manage the credentialing lifecycle efficiently, ensuring providers are enrolled and ready to bill without disruptions.
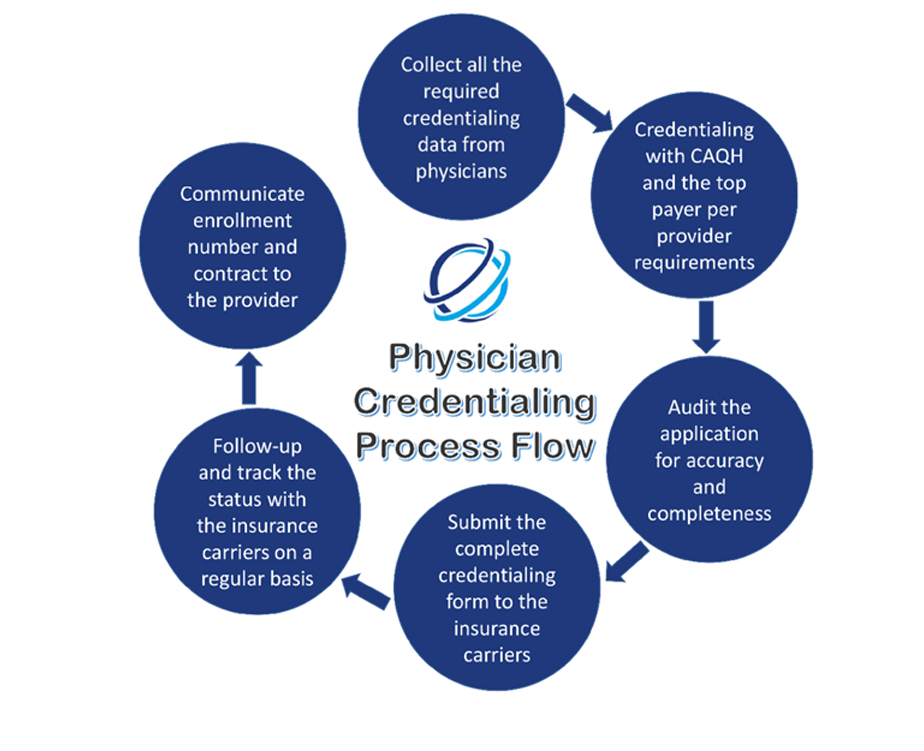
Our Process Includes:
Delays in credentialing can significantly impact a practice’s revenue cycle and operational efficiency. Our streamlined approach ensures that new providers are enrolled quickly, and existing providers remain compliant.
Benefits of Timely Enrollment.
AllegianceRCM delivers accurate, compliant, and efficient provider enrollment and credentialing solutions. Our expert-driven approach ensures that your claims are submitted correctly the first time—boosting cash flow and protecting your practice from regulatory risks.
We are technology agnostic and have worked on all modern SaaS based electronic medical records and practice management systems. The following is a list of most common practice management systems used across the industry and extensively used by us. If you don’t see your EHR here, please contact us.













