We simplify revenue cycle management with precision, expertise, and cutting-edge technology. Whether you’re an independent provider or a hospital group, we optimize financial workflows, reduce denials, and improve collections—so you can focus on patient care while we maximize your revenue.
The ever-evolving US healthcare system presents denial management hurdles, administrative overload, and revenue leakage—but you don’t have to navigate these challenges alone. AllegianceRCM ensures seamless financial administration, reduces claim rejections, and keeps your revenue cycle moving efficiently.
How We Help You Succeed?
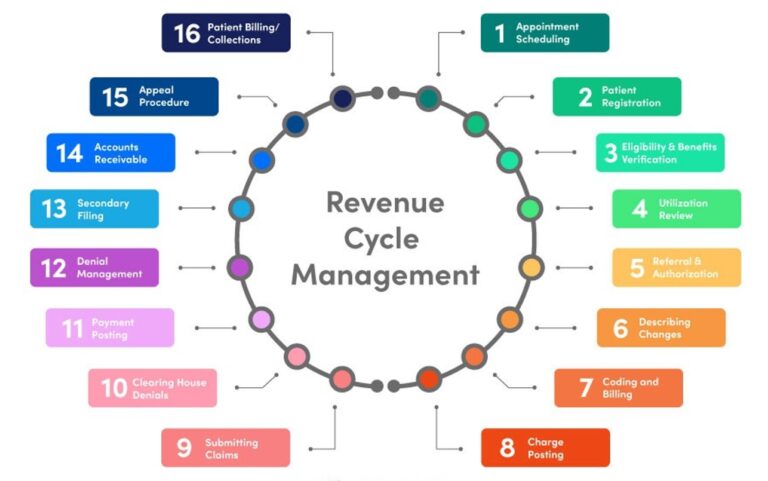
Optimize your practice’s revenue cycle with our end-to-end billing solutions. From patient intake to claims reimbursement, we ensure accuracy, compliance, and maximum reimbursements. Our specialized approach minimizes denials, enhances documentation, and streamlines operations—allowing you to focus on delivering exceptional patient care.
We answer patient calls and register new patients and also scheduled appointments. We verify Accurate patient information and complete insurance verification as it’s the foundation of smooth revenue cycle. We verify coverage, copays, deductibles, and prior authorizations upfront to prevent claim denials and payment delays, ensuring seamless billing from the start.
The mid-cycle is crucial for revenue integrity, covering coding, charge capture, and claim validation. We optimize each step to ensure compliance, accuracy, and timely reimbursements, reducing denials and revenue leakage. Our proactive approach guarantees precise documentation, minimizing financial risks and improving cash flow.
The back-end RCM process focuses on payment posting, denial resolution, and collections. Our streamlined workflows ensure faster reimbursements, minimize revenue loss, and optimize cash flow. With a dedicated AR management team, we handle outstanding claims efficiently, reducing aging accounts and maximizing revenue potential for healthcare providers.
Our advanced analytics provide deep financial insights, helping providers make data-driven decisions. We ensure regulatory compliance with HIPAA, CMS, and payer guidelines, preventing audits and penalties. Real-time reporting and predictive modeling enhance operational efficiency, optimize reimbursements, and drive financial success in an evolving healthcare landscape.
Partnering with AllegianceRCM for revenue cycle management ensures greater financial stability, reduced administrative burden, and optimized reimbursements. Our expertise helps healthcare providers increase collections, reduce denials, and improve patient satisfaction, allowing them to focus on delivering quality care while we handle the complexities of the revenue cycle.

Reduce overhead costs by eliminating in-house billing inefficiencies.
Stay compliant with ever-changing healthcare regulations and payer policies.
Optimize claims processing with minimal errors and proactive denial management.
Whether you’re a solo provider or a large group, we tailor solutions to fit your needs.
Gain real-time insights into financial performance and operational bottlenecks.
From patient registration to final collections, we manage the entire revenue cycle.
Transparent billing processes enhance trust and patient satisfaction.
A single point of contact ensures seamless communication and personalized service.