Specialty medical groups face unique revenue cycle challenges—from complex coding to evolving payer requirements. We provide specialized RCM solutions tailored to your specialty’s needs, ensuring higher reimbursements, faster claims processing, and reduced denials—so you can focus on what matters most: delivering exceptional patient care.
🚀 Partner with AllegianceRCM and experience the difference!
Multi-specialty and hospital-based specialty groups juggle diverse billing protocols, payer policies, and revenue cycle complexities across departments. At AllegianceRCM, we streamline revenue administration, coding accuracy, and compliance while ensuring seamless coordination across specialties. Our expertise in multi-specialty billing, hospital-affiliated reimbursements, and operational efficiency helps you reduce revenue leakage, optimize collections, and maintain financial stability—so your group can focus on patient care without administrative burdens.
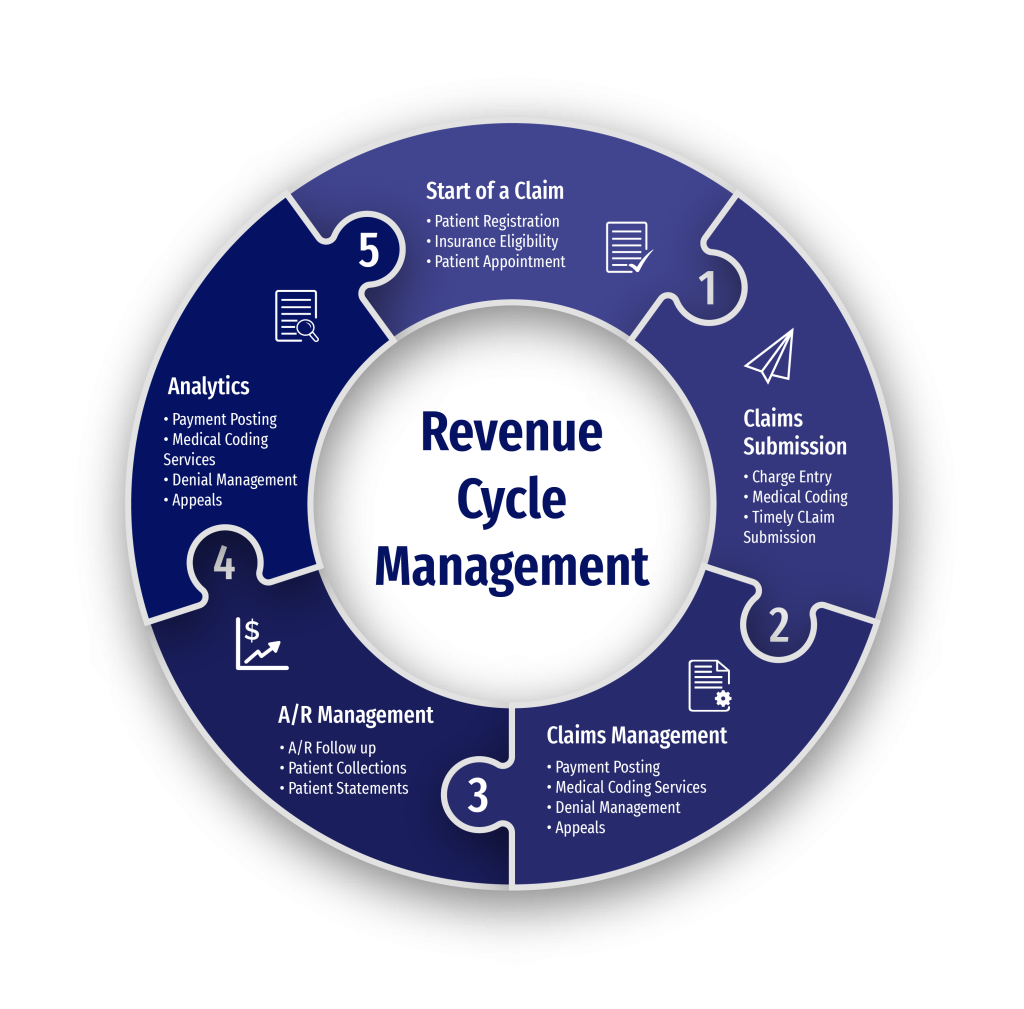
Optimize your practice’s revenue cycle with our end-to-end billing solutions. From patient intake to claims reimbursement, we ensure accuracy, compliance, and maximum reimbursements. Our specialized approach minimizes denials, enhances documentation, and streamlines operations—allowing you to focus on delivering exceptional patient care.
Accurate patient information and insurance verification are the foundation of a smooth revenue cycle. We verify coverage, copays, deductibles, and prior authorizations upfront to prevent claim denials and payment delays, ensuring seamless billing from the start.
Precise coding is essential for proper reimbursements. Our expert coders are AAPC certified with decades of experience to ensure accurate CPT, ICD-10, and HCPCS coding while adhering to payer-specific guidelines, reducing denials and optimizing claim success.
Submitting error-free claims is key to fast reimbursements. Our system scrubs each claim for errors before submission, ensuring compliance with payer rules, reducing rejections, and accelerating payments. We curate workflows with meticulous details to achieve higher clean claim ratio.
Our expert team of specialists proactively addresses denials with root-cause analysis, strategic appeals, and payer follow-ups, ensuring revenue recovery and claim success. We also specialize in underpayment recovery and handling significantly old A/R to do a final run before adjustments.
Our expert payments team ensure accurate payment posting by reconciling received payments against expected reimbursements. This step identifies underpayments, denials, and discrepancies, enabling quick corrective actions in time, on time, every time.
We streamline patient statements, payment plans, and collections while maintaining a positive patient experience, ensuring outstanding balances are resolved efficiently. Our trained reps help with you soft-collection efforts before moving to collection agency.
We are technology agnostic and have worked on all modern SaaS based electronic medical records and practice management systems. The following is a list of most common practice management systems used across the industry and extensively used by us. If you don’t see your EHR here, please contact us.














Let’s discuss how we can enhance your billing efficiency and maximize reimbursements. During your consultation, we’ll cover:
At AllegianceRCM, we assign a dedicated RCM Facilitator to every independent provider—a single point of contact ensuring seamless communication, expert guidance, and operational efficiency. From onboarding to compliance, this professional ensures your revenue cycle runs smoothly, allowing you to focus on patient care.

Our RCM Facilitator leads the transition process, ensuring seamless project onboarding, knowledge transfer, and training for your team. They oversee process execution, monitor key performance indicators, and implement best practices to enhance efficiency and maximize revenue.
With deep expertise in payer regulations, coding updates, and industry best practices, your facilitator ensures compliance and prevents revenue leakage. Through continuous audits, performance tracking, and real-time issue resolution, they help you achieve sustainable financial success.
📈 20% Faster Onboarding – Streamlined transitions with structured implementation
💰 15% Increase in Collections – Optimized claims management and payment follow-ups
⏳ 30% Reduction in Denials – Proactive compliance checks and coding accuracy
📞 24/7 Support & Guidance – A single point of contact for all RCM-related queries
✅ 100% Compliance Assurance – Regular audits and adherence to industry regulations
Stay informed with transparent and comprehensive monthly financial reports. We provide deep insights into claim performance, reimbursement trends, and revenue cycle efficiency, empowering you to make data-driven decisions that strengthen your practice’s financial health.